I’ve seen childbirth in this country go through some real changes. By the time I got involved, the childbirth revolution of the 60’s and early 70’s had already established (in most places) that women could have their husbands or partners with them in labor and delivery and they could choose not to be drugged; the birth of (forgive me) Natural Childbirth
In the later 80’s and 90’s, we childbirth educators were teaching expectant couples to beware the pitfalls of routine procedures like IVs, continuous fetal monitoring, artificial rupture of membranes, laboring in bed, pushing flat on one’s back, episiotomy, repeat cesarean section, and how to advocate for themselves.
The birth plan was created. We encouraged people to list their “preferences” around which birth procedures they wanted and which they wanted to avoid in advance of labor and delivery. Seems reasonable, right, not to have to have some discourse on the nature of episiotomy while you’ve got a human head pressing on your rectum?
Couples were hiring me as an advocate then; to make sure that the things they didn’t want done weren’t and that the things they did were. And I endeavored to do so without creating any conflict in the labor room, which was an industrious goal given hospital politics.
And while we worked so hard for and won the opportunity for women to create the childbirth experience of their choosing – doctor, midwife, hospital, birth center, home birth, unmediated, medicated and VBAC (vaginal birth after cesarean), there are a ton of mixed messages out there – from all sides.
In this medical/legal climate, we tell OB’s “We’re hiring you to give us a perfect baby and a perfect mother and if you don’t, we’ll sue you”. (This is partly how we all have come to make some sense of the fact that the practice of obstetrics in this country has become so industrialized and full of interventions.) The inherent message to expectant women is that the OB’s are not to be trusted.
The prevailing message from the childbirth community to expectant mothers is that natural birth, now referred to as “normal” birth, is the “best” birth. We’ve gone way beyond the great, International Childbirth Education Association’s (ICEA) slogan, “freedom of choice based on knowledge of alternatives”. The pressure on a pregnant woman today is to do so much research on childbirth before she has her baby that she could write a doctoral dissertation. And if she doesn’t, she is not being responsible. A woman needs to know all the risks and benefits before she makes any decisions (otherwise she can’t make an informed decision and that’s bad). She is to advocate for herself, even if she is not sure what she is to be advocating for or knows how to do so. A woman is irresponsible if she has a planned cesarean section or chooses an induction or an epidural, no matter how she arrived at that choice. We judge each other for how we give birth, how we parent, whether we stay at home or go back to work.
Here’s what I’m protesting now:
It’s unfair to presume that evidence based medicine means that it’s best practice for every one of us. It’s unfair to presume that every woman is in a place where she needs or wants or is capable at that time of “physiologic birth”. It’s unfair to presume that every woman needs or wants the “journey” and is better off for it. It’s unfair to promote that the best way to give birth is “normal” birth. Normal according to whom?
If we are really going to make a difference in maternity care in this country we have to ask and listen to what each individual mother needs to feel safe and secure. We need to respect each woman’s own perception of her threshold for pain and not presume that if she had only done enough research and/or had the ”right” support, she would do without medication. We need to meet each woman just where she is in her life and not dismiss her choices because she just doesn’t know how empowering a “normal” delivery is. We would emphasize that it is “better” to do whatever – breast feed, bottle feed, practice attachment parenting, let your baby cry it out, stay at home, go back to work, have your baby in daycare or in-home childcare, better to do anything because that individual mother has come to determine that it is better for her. We’d empower each woman by helping her figure out what she wants for herself and support her efforts to get there, not presume that we know what is better for her because we have the evidence based research to prove it.
We have to really listen. And to truly listen, I believe, is to do so without agenda, judgment or dogma.
The new revolution? It’s not really any different than the old one – it’s still about tolerance, respect and trust.

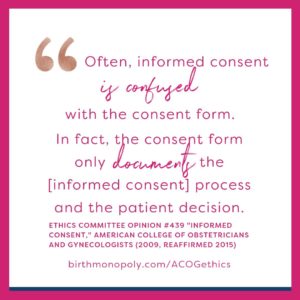 Here are a couple of examples (quoting Cristen here) of where care providers (maybe unaware of the legality) are violating your informed consent (which is often confused with the consent form). They present things as routine procedures and not optional:
Here are a couple of examples (quoting Cristen here) of where care providers (maybe unaware of the legality) are violating your informed consent (which is often confused with the consent form). They present things as routine procedures and not optional:


 From then on, when helping people prepare for their births, we talk a lot about staying flexible in order to make decisions that are aligned with your goals, especially when things aren’t going the way you imagined.
From then on, when helping people prepare for their births, we talk a lot about staying flexible in order to make decisions that are aligned with your goals, especially when things aren’t going the way you imagined.